Choosing when to have hair transplant surgery can determine the difference between natural-looking results and disappointing outcomes that require additional procedures. With up to 50% of men experiencing male pattern baldness and increasing numbers of women seeking hair restoration, understanding optimal timing has become crucial for successful hair transplant procedures.
The decision of when to get a hair transplant involves far more than simply noticing thinning hair or a receding hairline. Hair transplant surgeons emphasize that timing affects everything from the naturalness of results to the number of future procedures needed. Poor timing can lead to an unnatural appearance, wasted donor hair, or the need for multiple costly revisions.
This comprehensive guide examines the key factors that determine optimal hair transplant timing, from age considerations to hair loss stability requirements. Whether you’re in your twenties wondering if it’s too early or in your fifties concerned about age limits, understanding these timing principles will help you make an informed decision about hair restoration surgery.

Best Age for Hair Transplant Surgery
The optimal age range for hair transplant surgery typically falls between 30-45 years old for most hair transplant patients. This timing allows hair loss patterns to become more predictable and stable, while still maintaining adequate donor hair density and quality for successful transplantation.
Hair transplant specialists recommend that patients wait at least 5 years after initial hair loss onset before undergoing surgery. This waiting period helps ensure that the hair loss pattern has stabilized and won’t continue progressing rapidly after transplanted hair follicles are placed. During this time, many patients benefit from hair loss medications like finasteride and minoxidil to slow the hair loss process.
Early intervention between ages 25-30 may be possible if hair loss has clearly stabilized and shows a predictable pattern. However, younger patients face higher risks of needing additional procedures as their androgenetic alopecia continues to progress. Hair transplant surgeons often advise patience, particularly for patients experiencing severe hair loss at a young age.
Importantly, no upper age limit exists for hair transplant procedures if the patient maintains good health and has sufficient donor hair. Patients in their 50s, 60s, and even 70s can achieve successful results when they meet candidacy requirements and have realistic expectations about outcomes.
Key Factors That Determine Hair Transplant Timing
Several critical factors beyond age influence when to have hair transplant surgery. Understanding these elements helps determine individual readiness for hair restoration surgery and ensures optimal timing for natural looking results.
Hair loss stability represents the most crucial timing factor. The hair loss pattern should remain consistent for at least 12-18 months before considering hair transplantation. This stability indicates that aggressive hair loss has slowed, reducing the risk of continued balding around transplanted areas.
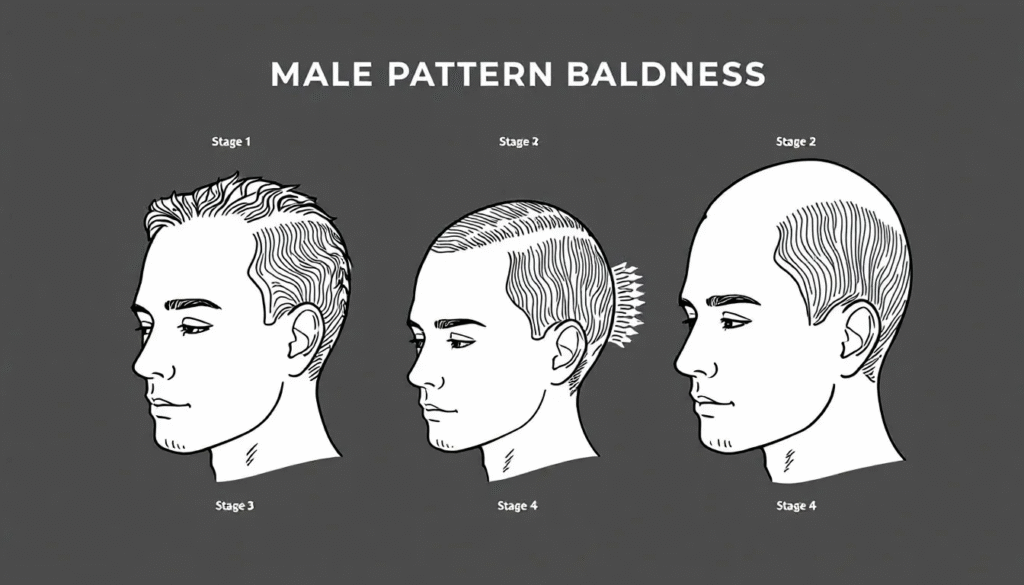
The extent and severity of current hair loss, often measured using the Norwood Scale for men, significantly impacts timing decisions. Different stages require varying approaches and may influence whether patients should delay surgery for medical treatments or proceed with transplantation.
Quality and quantity of donor hair available in the donor area determines both timing and expected outcomes. Patients with thick, healthy donor hair can proceed earlier with confidence, while those with limited donor hair may need to wait or consider alternative treatments.
The underlying cause of hair loss affects timing recommendations. Androgenetic alopecia follows predictable patterns suitable for transplantation, while temporary causes like stress, medications, or nutritional deficiencies should resolve before considering surgery.
Overall health status and surgical candidacy become increasingly important with age. Patients must be healthy enough to undergo surgery and follow the recovery process, which may require additional health assessments for older individuals.
Hair Loss Stabilization Requirements
Hair loss should demonstrate stability for at least 12-18 months before hair transplant surgery. This stabilization period allows hair transplant specialists to assess the true pattern of hair loss and predict future progression accurately.
Use of hair loss medications like finasteride and minoxidil often helps achieve stabilization by slowing the hair loss process. These treatments can preserve existing hair and provide a clearer picture of long-term hair loss patterns. Many hair restoration specialists require patients to try these medications before considering surgical intervention.
Avoiding surgery during active, rapid hair loss phases prevents disappointing results where newly transplanted hair appears isolated as surrounding hair continues to fall out. Patients experiencing sudden or aggressive hair loss should wait until the progression slows significantly.
Future hair loss patterns should be reasonably predictable based on family history, current pattern, and response to medications. This predictability helps hair transplant surgeons plan procedures that will look natural even as hair loss potentially continues in untreated areas.
Norwood Scale Considerations
The Norwood Scale provides a standardized way to assess male pattern baldness severity and determine appropriate timing for hair transplant procedures. Understanding these stages helps patients and surgeons make informed timing decisions.
Ideal timing usually occurs past Norwood Stage 3 for men, when the hair loss pattern becomes clearly defined. At this stage, patients have sufficient hair loss to justify surgery while retaining enough donor hair for successful transplantation.
Stages 1-2 may benefit more from hair loss treatment with medications rather than surgery. These early stages often respond well to finasteride and minoxidil, potentially delaying the need for surgical intervention by years.
Advanced stages 6-7 may present challenges due to insufficient donor hair for complete coverage. Patients at these stages require careful evaluation to determine if realistic results are achievable with available donor hair. Multiple sessions may be necessary, or patients may need to adjust expectations about final density.
Each stage requires different surgical approaches and graft counts. Early stages might need 1,000-2,000 hair grafts, while advanced stages could require 3,000-4,000 or more grafts across multiple sessions. Understanding these requirements helps with timing and financial planning.
Hair Transplant Timing by Age Group
Different age groups face unique considerations when determining optimal timing for hair transplant surgery. Understanding age-specific factors helps patients make informed decisions about when to proceed with hair restoration.
Hair Transplant in Your 20s
Hair transplant surgery is generally not recommended before age 25-30 due to the unpredictable nature of hair loss patterns in early adulthood. Hair loss patterns are not fully established in the early 20s, making it difficult to predict long-term results and plan appropriate treatment.
The risk of needing multiple future procedures increases significantly for younger patients. As androgenic alopecia continues to progress, patients who undergo hair transplant earlier may find their results looking increasingly unnatural as surrounding hair continues to thin.
Since 50% of men experience male pattern baldness, often starting in their late teens, many young patients feel urgency to address thinning hair. However, focusing on hair loss medications like finasteride and minoxidil during this period often provides better long-term outcomes by slowing progression and allowing patterns to stabilize.
Hair transplant specialists may consider surgery for patients in their late 20s only if hair loss has remained stable for 2+ years and follows a clearly defined pattern. Even then, patients must understand the high likelihood of needing additional procedures as they age.
Young patients should also consider that hair texture and density may change with age, potentially affecting how transplanted hair blends with natural hair over time. Waiting until the early 30s often provides more predictable and lasting results.
Hair Transplant in Your 30s and 40s
The 30s and 40s represent the peak age range for most successful hair transplant procedures. Hair loss patterns have typically stabilized by this time, allowing for more accurate treatment planning and better long-term results.
Patients in this age range usually have sufficient donor hair density and quality to achieve natural looking results. The hair follicles remain healthy and strong, leading to better graft survival rates and more robust hair growth after transplantation.
Better ability to predict long-term results makes this the ideal age for a hair transplant. Surgeons can more accurately assess how much more hair loss may occur and plan procedures accordingly, reducing the likelihood of needing major revisions.
Overall health is generally optimal for surgical procedures during this age range. Patients typically heal faster and experience fewer complications compared to older individuals. The recovery time is usually shorter, allowing patients to return to normal activities more quickly.
Hair transplant patients in their 30s and 40s also tend to have more realistic expectations and better understanding of the recovery process. This maturity often leads to higher satisfaction rates and better compliance with post-operative care instructions.
Hair Transplant After Age 45
No specific age limit exists for hair transplant surgery if patients maintain good health and have adequate donor hair. Many successful procedures have been performed on patients in their 50s, 60s, and beyond, proving that age alone doesn’t disqualify candidacy.
Patients over 45 may require additional health assessments, including EKG and comprehensive medical evaluation, to ensure they can safely undergo surgery. These evaluations help identify any conditions that might affect healing or increase surgical risks.
Hair density and quality may be reduced with age, potentially affecting both donor and recipient areas. Older patients might need to adjust expectations about achievable density, though natural looking results remain possible with appropriate planning.
Recovery time may be slightly longer for older patients, though most still heal well with proper care. Following post-operative instructions becomes even more important to ensure optimal healing and results.
The risk of waiting too long includes having insufficient donor hair for desired coverage. Patients who delay too long may find their donor area has thinned significantly, limiting transplant options and achievable results.

When to Try Alternative Treatments First
Several situations warrant trying non surgical treatments before proceeding with hair transplant surgery. Understanding when to delay surgery can save patients time, money, and ensure better eventual outcomes when surgery becomes appropriate.
Early stages of hair loss, particularly Norwood stages 1-2, often respond well to medications and may not require surgical intervention for years. Starting with finasteride, minoxidil, or other hair loss treatment options allows patients to slow progression and potentially delay surgery until patterns stabilize.
Patients under 25-30 years old should generally explore non-surgical options first unless hair loss has been clearly stable for multiple years. Young patients have the most to gain from preventing hair loss and the most to lose from premature surgery.
Recent onset hair loss within the past 2 years warrants a conservative approach. Sudden hair loss may be temporary or related to stress, medications, or medical conditions that resolve with time or treatment.
Temporary hair loss from stress, medication side effects, or illness should be addressed by treating the underlying cause rather than surgery. Once the trigger is removed and hair has had time to recover, patients can reassess their need for transplantation.
Insufficient donor hair quality or quantity makes surgery inadvisable regardless of age. Patients with thin, weak donor hair or limited donor area should focus on preserving what they have rather than risking poor surgical outcomes.
Effective Pre-Transplant Treatments
Finasteride (Propecia) blocks DHT production and can significantly slow hair loss progression in most men. This medication helps stabilize hair loss patterns and preserve both existing hair and potential donor hair for future transplantation.
Minoxidil stimulates hair growth and can improve hair density in both men and women. Applied topically twice daily, it often provides modest regrowth and helps maintain existing hair during the observation period before surgery.
Lifestyle modifications including stress reduction, healthy diet, and regular exercise support overall hair health. While these changes won’t reverse genetic hair loss, they optimize conditions for both natural hair retention and post-surgical healing.
Nutritional support with vitamins and supplements may help address deficiencies that contribute to hair loss. Iron, vitamin D, and biotin deficiencies can worsen hair loss and should be corrected before considering surgery.
The recommended timeline involves trying these medications for 12-18 months before considering surgery. This period allows treatments to reach full effectiveness and provides time to assess hair loss stability. Patients who respond well to medications may choose to delay surgery indefinitely.
Individual Candidacy Factors Beyond Age
Several individual factors beyond age significantly influence hair transplant timing and candidacy. A thorough assessment of these elements helps determine whether patients are ready for surgery and what results they can realistically expect.
Hair Density and Thickness Evaluation
The donor area must contain sufficient healthy hair follicles to achieve natural looking results in the recipient area. Hair transplant surgeons carefully evaluate donor density, typically requiring at least 2-2.5 follicular units per square centimeter for successful transplantation.
Thick hair requires fewer grafts than thin hair to achieve the same visual density. Patients with coarse, thick hair often achieve better coverage with fewer transplanted hair follicles, making them excellent candidates for surgery at an earlier stage.
Hair density naturally decreases with age, favoring earlier procedures when donor hair is at its peak quality. Younger patients with thick, dense donor hair often achieve superior results compared to older patients with thinner donor areas.
Curly or Afro-Caribbean hair textures often provide better visual coverage due to their natural volume and curl pattern. These hair types can create the appearance of greater density with fewer actual hair grafts, potentially making patients good candidates even with modest donor areas.
Hair transplant specialists use specialized tools to measure donor density and project how many grafts can be safely harvested. This assessment helps determine whether single or multiple sessions will be needed and what level of coverage is achievable.
Extent of Hair Loss Assessment
Limited donor hair availability means that patients with extensive hair loss may only be able to restore priority areas like the hairline and crown. Understanding these limitations helps set realistic expectations and determine if timing is appropriate.
Severe baldness classified as Norwood stages 6-7 may not be suitable for complete restoration with current hair transplant techniques. Patients at these advanced stages need careful evaluation to determine if meaningful improvement is possible with available donor hair.
Multiple sessions may be necessary for extensive hair loss, requiring patients to plan for procedures spread across several years. This timeline affects both financial planning and expectations about when final results will be achieved.
Realistic expectations based on available donor hair become crucial for patient satisfaction. Hair restoration specialists help patients understand what level of improvement is possible and whether their goals align with biological limitations.
The hair loss pattern also influences timing decisions. Patients with aggressive, rapidly progressing hair loss should wait for stabilization, while those with slow, predictable progression may proceed with surgery sooner.

Signs You’re Ready for Hair Transplant
Several key indicators suggest optimal timing for hair transplant surgery. Meeting these criteria increases the likelihood of successful outcomes and patient satisfaction with results.
Hair loss stability for 12+ months despite treatment indicates that the pattern has established and is unlikely to change dramatically after surgery. This stability provides confidence that transplanted areas won’t become isolated as surrounding hair continues to fall out.
Reaching the minimum age of 25-30, preferably 30+, ensures that hair loss patterns have had time to establish fully. Patients in this age range face lower risks of dramatic pattern changes that could affect surgical outcomes.
Adequate donor hair density and quality in the donor site provide the foundation for successful transplantation. Patients should have thick, healthy hair in the donor area with sufficient density to harvest the needed number of grafts.
Realistic expectations about hair transplant results prevent disappointment and ensure satisfaction with outcomes. Patients should understand that surgery restores hair to balding areas but doesn’t prevent future hair loss in untreated regions.
Good overall health for surgery includes absence of conditions that impair healing or increase surgical risks. Patients should be able to follow post-operative care instructions and have adequate time for proper recovery.
Financial readiness for the procedure, typically ranging from $4,000-$15,000 depending on the extent of surgery, ensures patients can complete their planned treatment without financial stress affecting their decisions.
The ability to follow post-operative care instructions, including avoiding direct sunlight, limiting physical activity, and attending follow-up appointments, is essential for optimal healing and results.
Understanding that results take 9-12 months to fully develop helps patients maintain realistic timelines and avoid premature concerns about hair growth progress.
Professional Consultation and Timing Assessment
Professional evaluation by qualified hair transplant specialists provides the most accurate assessment of individual timing and candidacy. These consultations examine multiple factors that influence optimal timing decisions.
Hair transplant surgeons assess individual hair loss patterns using standardized classification systems and predict likely progression based on family history, current pattern, and response to treatments. This analysis helps determine whether timing is optimal or if patients should wait longer.
Digital imaging technology allows surgeons to model potential results and show patients what they can realistically expect from surgery. These simulations help with timing decisions by demonstrating whether current hair loss warrants surgical intervention.
Graft calculators help estimate the number of hair follicles needed to achieve desired results. This information influences timing by showing whether sufficient donor hair is available and how many sessions might be required.
Discussion of FUE (follicular unit extraction) versus FUT techniques based on patient age, goals, and hair characteristics helps optimize surgical planning. Younger patients might prefer FUE for less visible scarring, while older patients might benefit from FUT’s higher yield.
Timeline planning for optimal results includes coordinating surgery with patient schedules, ensuring adequate recovery time, and planning any necessary follow-up procedures. Surgeons help patients understand the complete timeline from consultation to final results.
Most reputable hair restoration specialists offer free consultations to assess candidacy and timing. These evaluations provide personalized recommendations without financial pressure, allowing patients to make informed decisions about when to proceed.
Hair transplant specialists also coordinate with dermatologists and other medical professionals to ensure any underlying conditions are properly managed before surgery. This comprehensive approach optimizes both timing and outcomes.
The consultation process typically includes examination of the donor area, assessment of hair loss progression, discussion of goals and expectations, and development of a personalized treatment plan with optimal timing recommendations.

Understanding when to have hair transplant surgery requires careful consideration of multiple factors beyond simple age requirements. The optimal timing balances hair loss stability, adequate donor hair availability, realistic expectations, and individual health status.
Most patients achieve the best results when they wait for hair loss patterns to stabilize, typically by age 30 or after at least 5 years of pattern hair loss. This patience often prevents the need for multiple procedures and ensures more natural, lasting results.
However, individual circumstances vary significantly, making professional consultation essential for accurate timing assessment. Hair transplant surgeons can evaluate your specific situation, predict likely outcomes, and recommend optimal timing based on your unique hair loss pattern and goals.
The investment in proper timing pays dividends in better results, fewer revision procedures, and higher long-term satisfaction. Whether you’re in your twenties considering early intervention or in your fifties wondering about age limits, understanding these timing principles helps ensure you make the right decision for your individual situation.
If you’re considering hair restoration surgery, schedule a consultation with a qualified hair transplant specialist to discuss your specific timing needs and develop a personalized treatment plan that optimizes your chances of achieving natural looking results.